Home » Orthopedic Surgeon Services » Knee » Total Knee Replacement
Total Knee Replacement
Arizona Orthopedic Surgery Solutions for Total Knee Replacement
Complete Knee Replacement Educational Video
Knee Arthritis & Knee Replacement Diagnosis Video
Knee Arthritis & Knee Replacement Treatment Video
Cori Navigation Total Knee Video
Total Knee Replacement Treatment
In many areas, elective orthopedic procedures postponed due to COVID-19 have resumed.
A severely damaged knee by arthritis or injury will make it difficult to perform basic activities like walking or climbing stairs. You might even have pain while you are sitting or lying down.
If nonsurgical treatments like medications and walking supports are no longer helpful, you may consider total knee replacement surgery. Joint replacement surgery is a safe and
an effective procedure to relieve pain, resume normal activities, and correct leg deformity.
In 1968 the first knee replacement surgery was first performed. Since then, advancements in surgical materials and techniques have significantly increased their effectiveness. Thankfully, total knee replacements are one of the most successful procedures. In 2017, The Agency for Healthcare Research and Quality estimates more than 750,000 knee replacements were performed in The United States.
Whether you are just exploring treatment options or have already decided to have total knee replacement surgery, this article will help explain more about this valuable surgery.
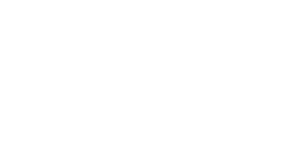
Anatomy
The knee is the biggest joint in the body. Having healthy knees is necessary to perform most everyday activities.
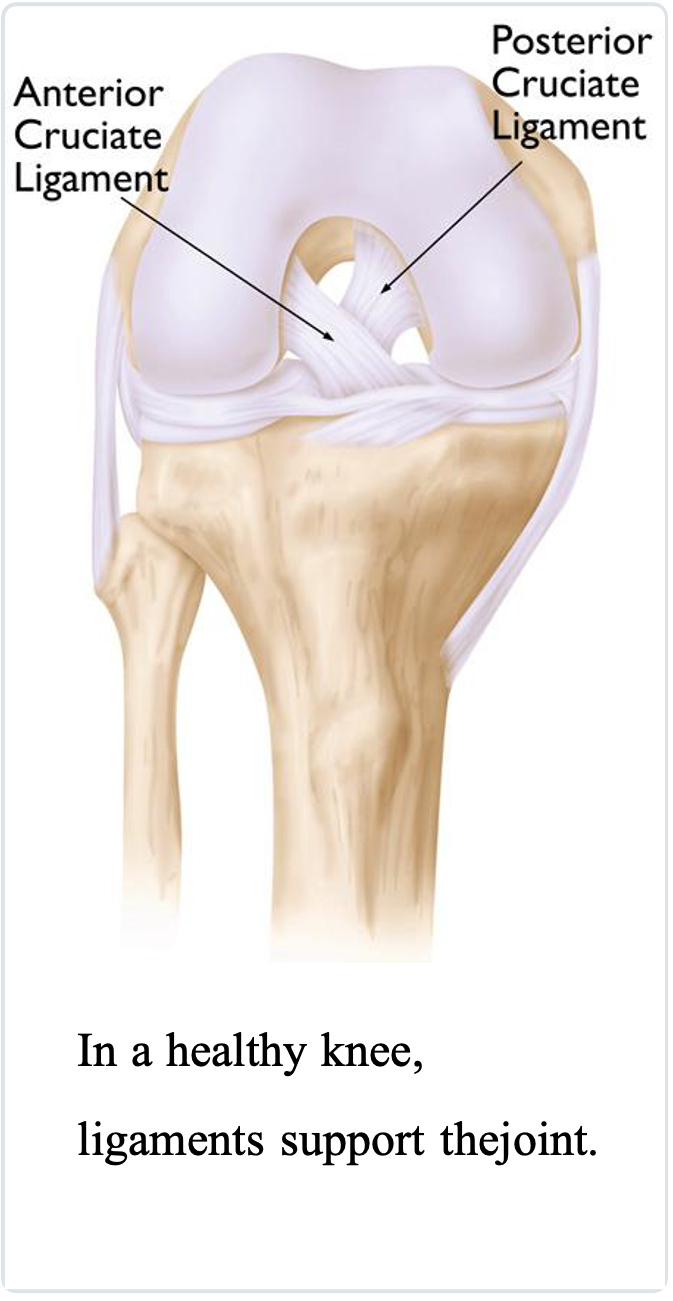
The knee joint is made of the upper end of the shinbone (tibia), the lower end of the thighbone (femur), and the kneecap (patella): articular cartilage, a smooth coating on the surface of these three bones. The cartilage protects the bones and enables them to move effortlessly within the joint. Menisci are shock absorber structures located between the femur and tibia. These C-shaped wedges cushion the joint. Ligaments provide stability and hold the knee together. The thigh muscles give the knee strength.
The remaining surfaces of the knee are covered by a thin lining called the synovial membrane. This synovium releases a fluid that lubricates the cartilage, reducing friction to nearly zero in a healthy knee. Usually, these components work in harmony. But knee arthritis can disrupt this harmony, resulting in reduced function and pain.
Cause
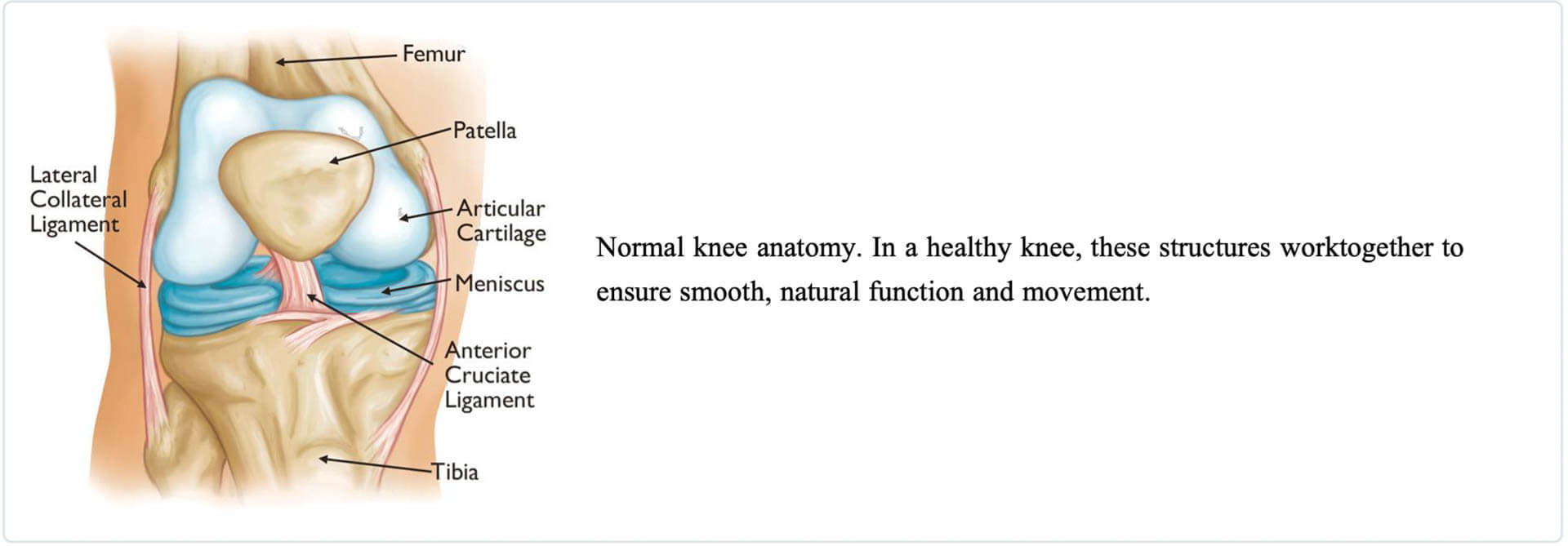
The most common reason for persistent knee pain and disability is arthritis. The three most common types of knee arthritis are osteoarthritis, rheumatoid arthritis, and post-traumatic arthritis.
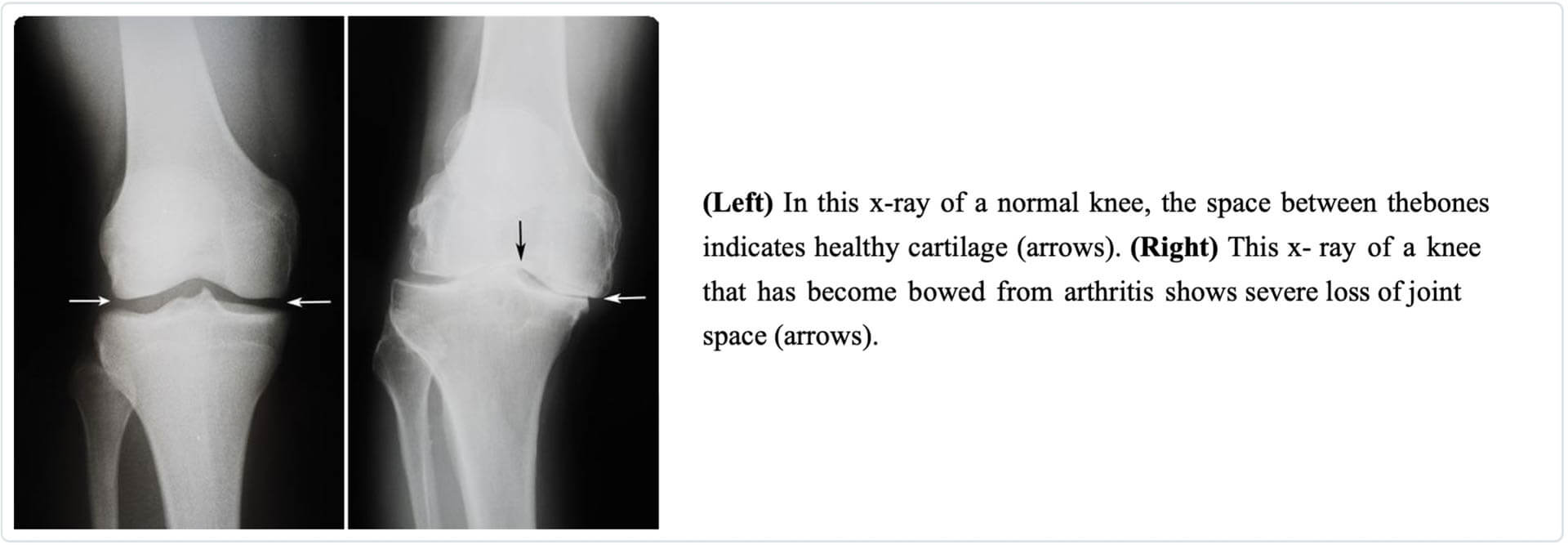
Osteoarthritis. The cartilage is a soft layer that lines and cushions the bones of the knee, degrades, and wears away. This is age-related “wear and tear” mostly in people 50 years of age and older but can occur in younger people, too. The bones then painfully grind against one another, resulting in knee stiffness and discomfort.
Rheumatoid arthritis. This is the most common form of “inflammatory arthritis.” This is a condition in which the synovial membrane that surrounds the joint becomes thickened and inflamed. Chronic inflammation damages the cartilage and ultimately causes cartilage loss, pain, and stiffness.
Post-traumatic arthritis. Fractures (broken bones) surrounding the knee or tears of the ligaments damage the articular cartilage over time, limiting knee function and causing pain.
Description
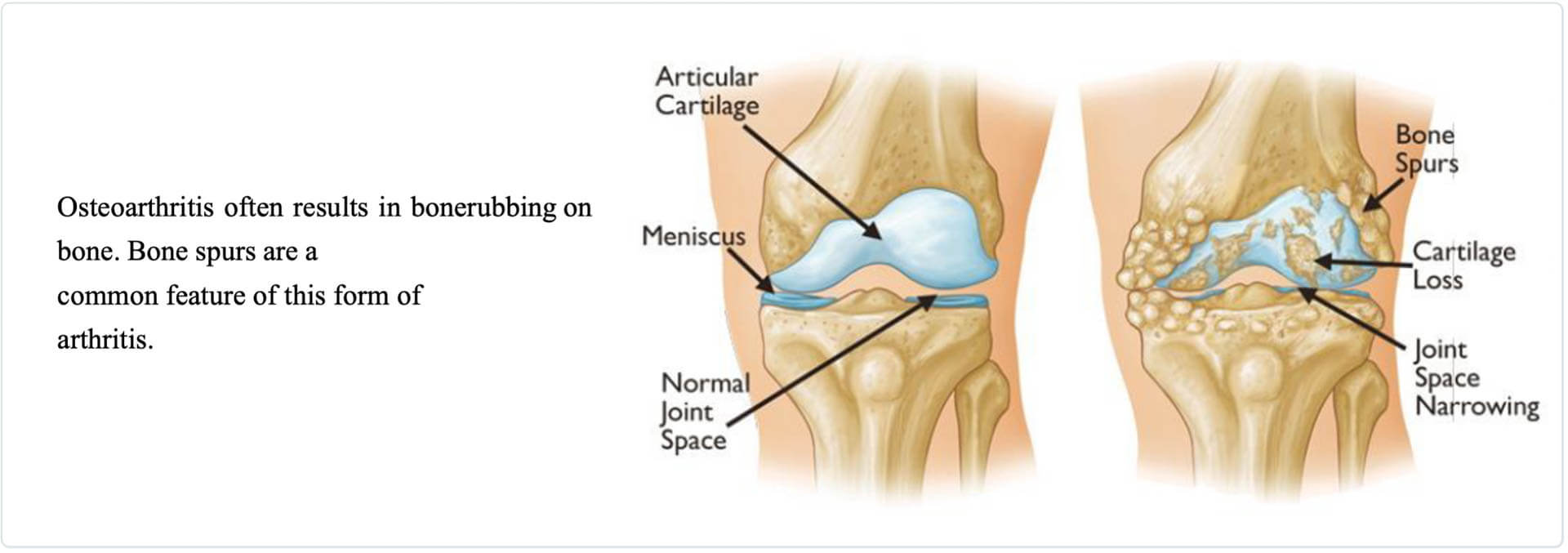
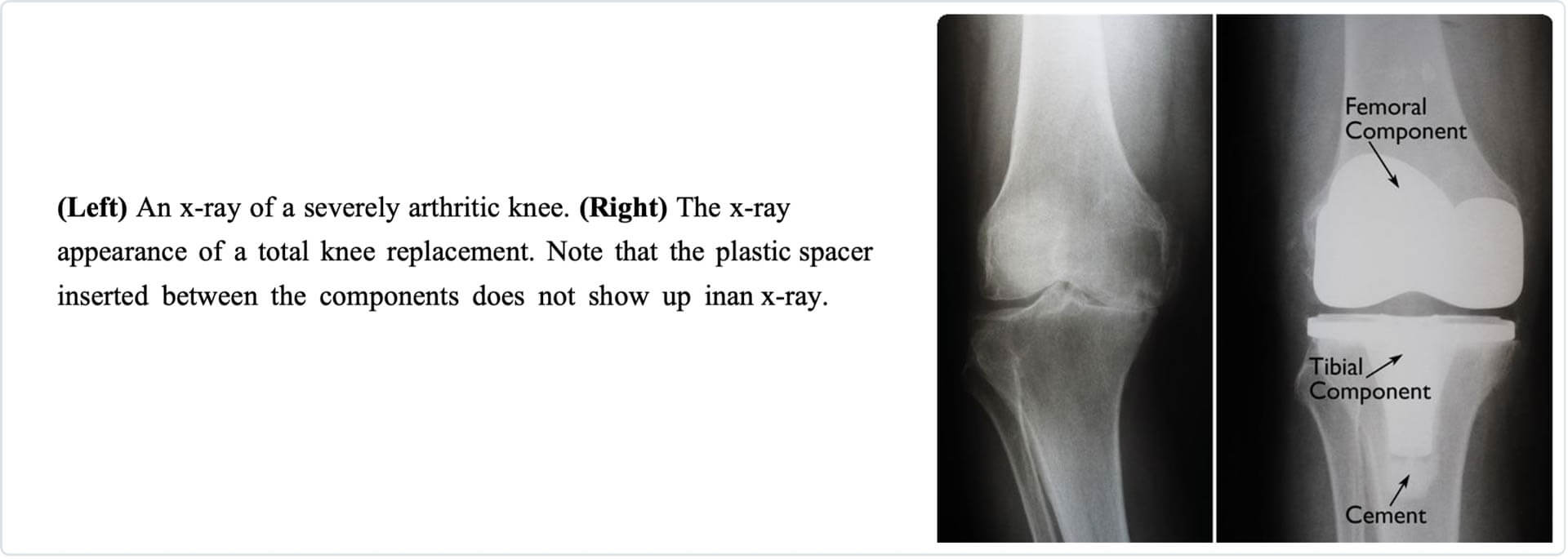
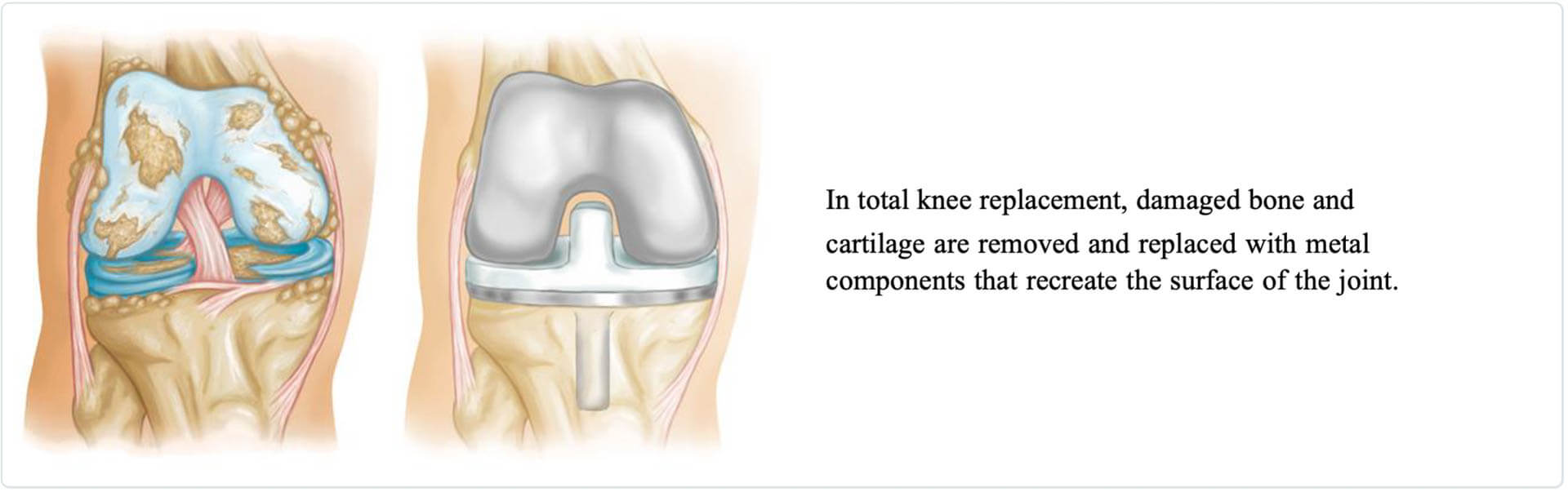
A knee replacement (also called knee arthroplasty) is more accurately called a knee “resurfacing” because only the surface of the bones is replaced.
There are four basic steps during knee replacement surgery:
- Prepare the Remove damaged cartilage surfaces at the ends of the femur and tibia
- Position the metal The exposed bone surface is replaced with metal components that recreate the joint. These metal implants may be cemented or “press-fit” into the bone.
- Resurface the A plastic implant is added to the underside of the kneecap.
- Insert a A medical-grade plastic shock absorber is placed between the metal components resulting in a smooth gliding surface.
Is Total Knee Replacement for You?
The decision for surgery should be a cooperative one between you, your family, your primary care doctor, and Dr. George Gendy. Your doctor, friend, or family may recommend you to Dr. George Gendy for a thorough evaluation to determine if you benefit from total knee replacement.
When Surgery Is Recommended
There are many reasons why Dr. George Gendy may recommend knee replacement surgery. People who benefit from total knee replacement have:
- Severe knee pain or knee stiffness limits daily activities, including walking, getting in and out of chairs, and climbing stairs. Arthritic knee pain may cause difficulty walking more than a few blocks without significant pain or the need to use a walker or cane.
- Moderate or severe knee pain while resting, day or night
- Chronic knee pain and swelling that persists despite rest or medications.
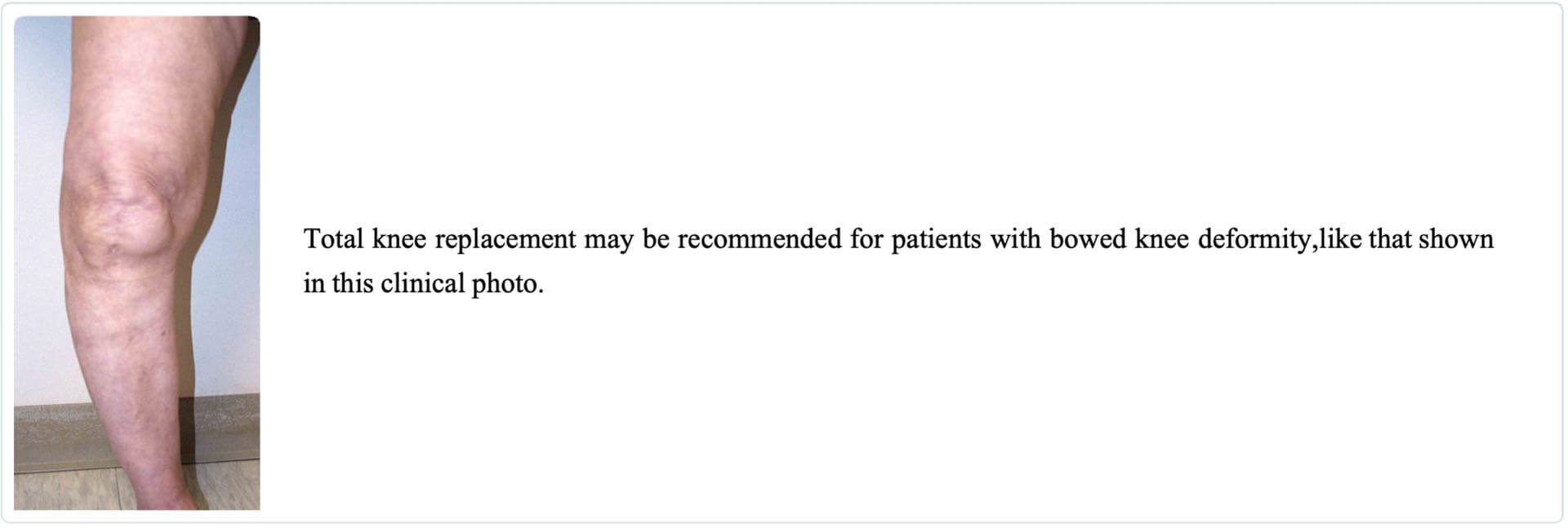
- Knee deformity — a bowing out or bowing in of the knee
- Failure to substantially decrease knee pain with other treatments such as anti-inflammatory medications, physical therapy, cortisone injections, lubricating injections, or other surgeries
Candidates for Surgery
There are no firm age or weight restrictions for total knee replacement surgery. However, your body mass index (BMI) should be less than 35 ideally. Recommendations for surgery are based primarily on pain and disability rather than age. Many people who undergo total knee replacement are age 50 to 80, but Dr. George Gendy evaluates patients individually. Total knee replacements are performed successfully at both middle and elderly ages with degenerative arthritis.
The Orthopaedic Evaluation
An evaluation with George Gendy MD consists of several components:
- Medical Dr. George Gendy will gather information about your health, your knee pain, and your ability to function.
- Physical This will include knee motion, strength, stability, and leg alignment.
- X-rays. These pictures help determine the extent of damage and deformity in your
- Other Sometimes blood tests or cutting-edge imaging, such as a magnetic resonance
- imaging (MRI) scan, are needed to evaluate the status of the bone and soft tissues of your knee.
Dr. George Gendy will review the results with you and discuss whether total knee replacement surgery is the best method to improve your function and relieve your pain. Other treatment options — including physical therapy, medications, injections, or different types of surgery — will also be considered and discussed.
In addition, Dr. George Gendy will explain the potential risks and complications of total knee replacement, including those during and after your surgery.
Choosing to Have Knee Replacement Surgery
Realistic Expectations
An important factor in deciding to have total knee replacement surgery is understanding what the procedure can and cannot do.
Most people with total knee replacements experience a dramatic reduction of knee pain and a substantial improvement in performing daily tasks. However, total knee arthroplasty will not allow you to do more than you could before you developed arthritis.
With regular use and activity, each knee replacement implant begins to wear its plastic spacer. Excessive activity or weight speeds up this normal wear and causes the knee replacement to loosen. Loose implants become painful over time. Therefore, most surgeons discourage high-impact activities such as jumping, jogging, running, or other high-impact sports after a knee replacement.
Realistic activities following total knee replacement include swimming, unlimited walking, golfing, driving, ballroom dancing, light hiking, biking, pickleball, tennis, and other low-impact sports.
With suitable activities, knee replacements can last for many years.
Potential Complications of Surgery
Thankfully the complication rate after a total knee replacement is low. Major complications, such as deep joint infection, occur in fewer than 2% of patients. Complications such as stroke or heart attack occur even less frequently. Although uncommon, when major complications occur, they can prolong or limit full recovery.
Discuss your concerns thoroughly with Dr. George Gendy before your knee replacement surgery.
Infection. Infection may occur in the incision site or deep at the level of the joint replacement implants. It can happen within days or weeks of your surgery. However, it can also occur years later. Minor infections in the surgical site area are generally treated with antibiotics. Significant or deep infections may require additional surgery and removal of the metal implants. An infection in a different body part can spread to your joint replacement.
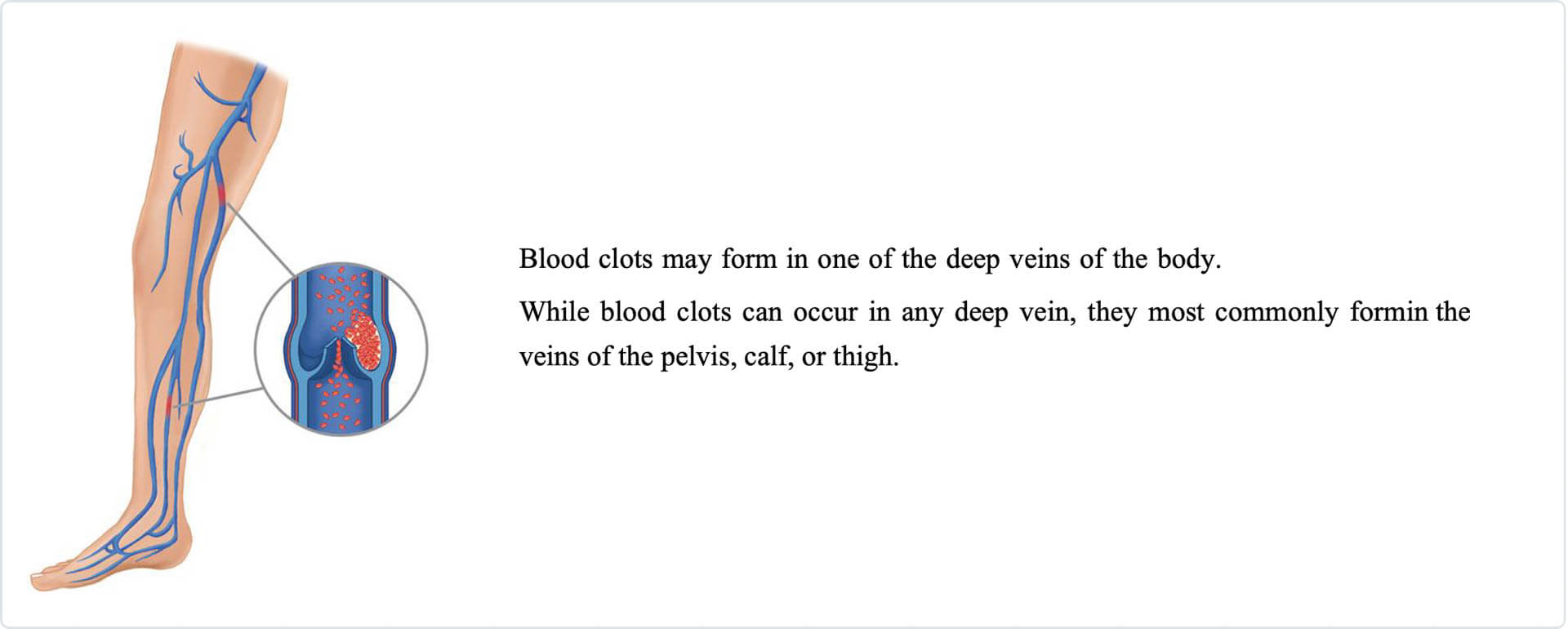
Blood clots. Blood clots are synonymous with deep vein thrombosis (DVT). DVTs are a well-known complication of knee replacement surgery. If a blood clot travels to your lungs, it is called a pulmonary embolism which can be life-threatening. Dr. George Gendy will outline a prevention program, which may include intermittent elevation of your legs, leg exercises to increase circulation, and clot preventing medication to thin your blood.
Pain. Although rare, some patients may have persistent knee pain after their replacement. This can come from the soft tissue around the knee, as the replacement only changes the bone and joint surface but not the soft tissue around the knee. Thankfully, most patients experience excellent pain relief after their knee replacement.
Knee stiffness. Projected knee bending averages 115° of knee flexion (bending) after surgery; however, scarring of the knee can occasionally occur. Scarring may then limit knee bending, particularly in patients with minimal motion before surgery.
Neurovascular injury. While rare, damage to the nerves or blood vessels around the knee can occur during surgery.
Implant problems. Despite implant designs and surgical technique advancements, implant surfaces may wear down, and the components may loosen.
Preparing for Surgery
Medical Evaluation
When you elect to have total knee replacement surgery, Dr. George Gendy may ask you to schedule an examination with your doctor several weeks before the operation. This is needed to ensure you are at your healthiest to have knee replacement surgery and recovery. Chronic medical conditions, like heart disease or atrial fibrillation, may also be evaluated by a specialist, such as a cardiologist, prior to surgery.Tests
EKG, blood samples, and urine samples may be needed for your surgical clearance.Medications
Tell Dr. Gendy about the medications you are taking. Dr. Gendy will tell you which medicines to stop or continue taking before your knee replacement surgery.Urinary Evaluations
If you have a history of recent or frequent urinary infections should have a urological evaluation before your knee replacement. Dr. Gendy recommends older men complete their required prostate treatment before knee replacement.Dental Work
Even though the risk of infection after knee replacement is shallow, an infection can occur if dental bacteria enter your bloodstream. To reduce the risk of infection:- You must avoid ANY dental work (including a routine dental cleaning) for 2 WEEKS before surgery.
- Gendy prefers all planned dental work to be completed well before surgery unless it can be delayed 6 MONTHS after surgery.
Social Planning
Although you can walk with a cane, crutches, or a walker soon after surgery, you will need assistance for several weeks with such tasks as showering, cooking, shopping, and laundry. If you live alone, our team can assist with advance arrangements to have someone help you at home. If an extended care facility works best for you, we can arrange for a short stay for your recovery.Home Planning
Modifications can help your home easier to navigate during your recovery. The following items may assist with daily activities.- Safety bars in your shower
- Secure handrails along your stairways
- High chair for your early recovery with a firm seat cushion (and a height of 18 to 20 inches), two arms, and a footrest for leg elevation
- Raised toilet seat
- Shower bench or chair for bathing
- Remove loose carpets, runners, and loose cords
- A temporary bedroom space on the same floor to avoid difficulty walking up or downstairs during your early recovery
Your Surgery
On the day of your knee replacement, you will be admitted to the hospital or go home the same day. Discuss the plan to either be admitted or go home with Dr. George Gendy before your operation.
Anesthesia
The anesthesia team will evaluate you upon your arrival at the surgery center or hospital. General anesthesia, which is when you are put to sleep combined with a peripheral nerve block (an injection into the thigh to numb the knee), is commonly used. Alternative anesthesia includes spinal or epidural, in combination with a peripheral nerve block; this is when you are awake; however, you are numb from the waist down. With your input, the anesthesiologist will determine the best type of anesthesia.
Procedure
DURATION OR LENGTH OF SURGERY
The knee replacement usually takes 1 to 3 hours.
TECHNIQUE
Dr. George Gendy removes the damaged cartilage and bone with a robotic-assisted minimally invasive tool. The robot is an assist device tool that aids in confirming correct bone cuts, alignment, and placement of the implant. Similar to turn by turn GPS directions. This allows for minimally invasive knee surgery with more accurate bone cuts and implant placement for the optimal position.
After the bone cuts have been made, Dr. George Gendy then positions the metal and plastic knee replacement implants to restore the alignment and function of your knee.
Different types of implants are used to meet each patient’s needs.
AFTER SURGERY
You will be relocated to the post-anesthesia care unit (PACU), also known as the recovery room, for several hours, where you will recover from anesthesia. After you awake and recover from anesthesia, you will go to your hospital room or be discharged home.


Your Hospital or Surgery Center Stay
If admitted to the hospital, you may stay one to three days on average.
Pain Management
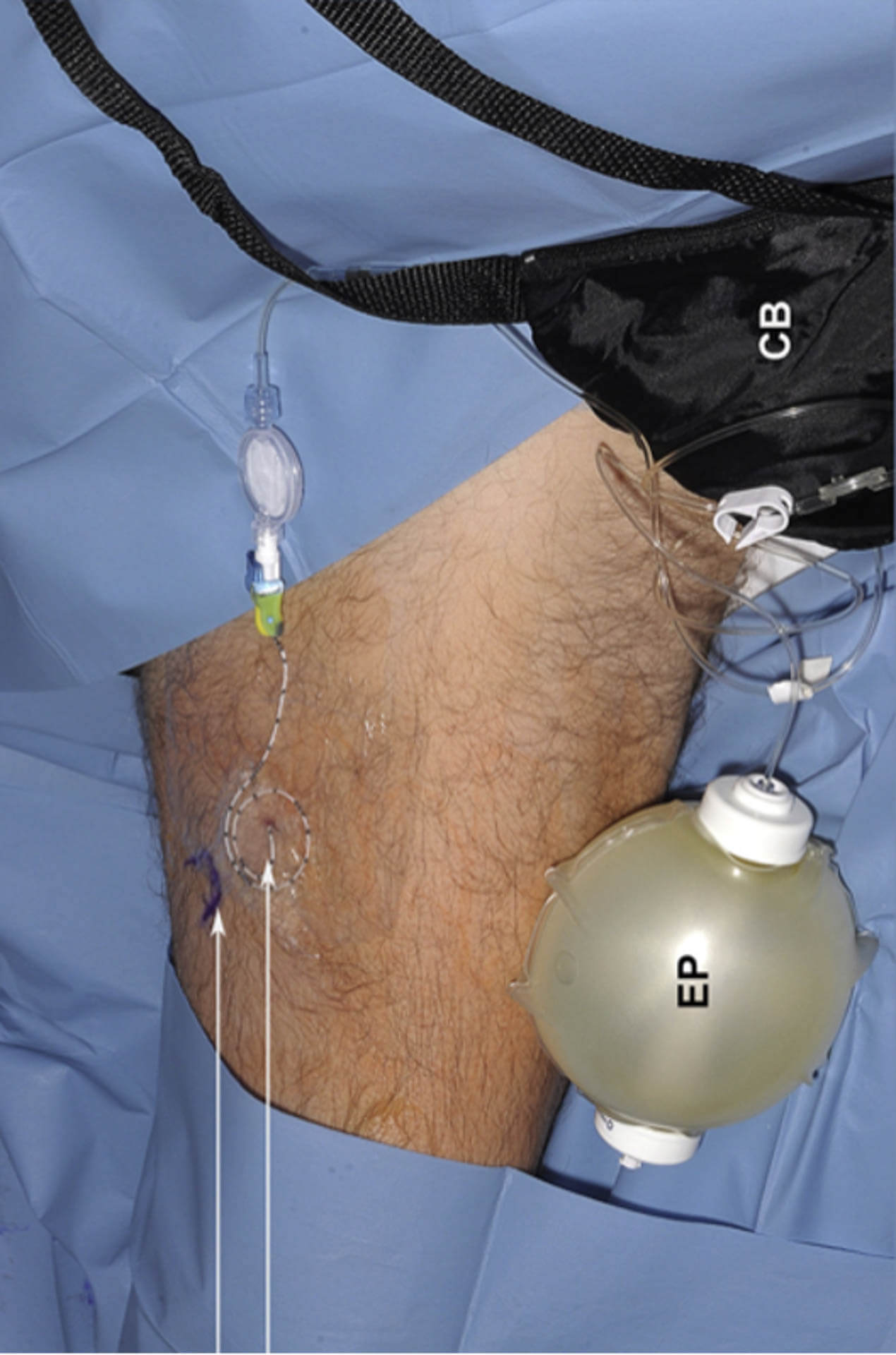
You will have a nerve block pump for approximately three days. This will greatly minimize your pain. The nerve block pump drips numbing medication into the thigh around the nerve that senses knee pain. As a result, you may only feel some pain. This decreased level of pain is a natural part of the healing process. Be aware that the pump lasts approximately three days when the pain may be at its greatest, and you will have the luxury of not experiencing as much pain because of the nerve block. However, once the block wears off, you may begin to notice an increase in pain.
Medications including nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen (Tylenol), and local anesthetics (nerve block with a pain pump) are often prescribed for short-term pain relief after surgery. Dr. Gendy may use a combination of these medications to improve pain relief to decrease the dependence on opioids.
Although opioids help relieve pain after surgery, be aware they are narcotic and can be
addictive. Narcotic dependency and overdose have become public health issues in the U.S.
Once the pain improves, stop taking opioids. Inform your doctor if the pain has not started to improve within a week of your surgery.
Blood Clot Prevention
Dr. George Gendy may prescribe one or more measures to prevent blood clots and decrease leg swelling. These may include support socks, inflatable leg pumps, and blood thinners.
Foot and ankle movement is also encouraged after surgery to increase blood flow in your leg muscles. Foot and ankle movements help prevent blood clots and swelling.
Physical Therapy
You will begin exercising your new knee hours after surgery. A physical therapist will meet you at the bedside and teach you leg strengthening and knee movement exercises to allow walking and other normal daily activities once you recover from anesthesia.
Preventing Pneumonia
It is common to have shallow breathing after surgery. This is usually because of anesthesia, pain medications, and increased time spent in bed. Persistent shallow breathing can lead to decreased airflow in the lungs called (termed “atelectasis”), making patients susceptible to pneumonia and fever. Take frequent deep breaths to help prevent pneumonia. You may be given a breathing device called a spirometer to encourage deeper breaths.


Your Recovery at Home
Follow Dr. George Gendy’s instructions at home to ensure a successful outcome.
Wound Care
Incision:
Your incision site is closed with an absorbable suture that is underneath the skin and does not need to be subsequentially removed. Therefore, you will not have visible stitches on the front of your knee. Dr. Gendy does not use staples.
Dressing
After surgery, a special bandage is placed that is good for approximately 7-14 days. This special bandage applies negative pressure that helps to reduce incision breakdown and infection.
This dressing helps reduce wound breakdown by 75% and surgical incision site infection by 50%.
Washing and showering
Light showering is allowed; however, the pump should be disconnected and placed in a safe place where it will not get wet. While disconnected, do not be expose the dressing to a direct spray or submerge the dressing in water. Maintain the end of the tubing attached to the dressing is facing down or cover it with a saran wrap so that water does not enter the tube.
Do not submerge (e.g., bathing or swimming) the wound in water until it has fully healed, sealed, and dried. This usually takes four weeks. You may continue to bandage the incision to prevent irritation from clothing or support stockings.
General activity
The PICO 7 sNPWT pump is carried in your pocket or belt clip; wherever is most comfortable for you. The pump should be accessible to check the status routinely.
Safety
The PICO pumps contain a MAGNET. Keep the PICO pumps at least 4 inches (10 cm) away from other medical devices at all times. As with all electrical medical equipment, failure to maintain appropriate distance may disrupt the operation of nearby medical devices.
Sleeping
Make sure that the PICO 7 sNPWT pump is somewhere safe and cannot be pulled off a table or cabinet onto the floor while sleeping.
Travel
Yes, you are allowed to travel on an aircraft, boat, and train with your PICO 7 sNPWT system.
Radiofrequency can affect the pump. If the PICO 7 pump malfunctions, change the batteries. Contact your healthcare professional if the error is not corrected.
Activity
Home exercise is a critical component of your recovery during the first six weeks.
Anticipate resuming most normal activities of daily living within 3 to 6 weeks following surgery. Some pain with movement and at night is common weeks after surgery.
Your exercise program should include:
- A progressive walking program to gradually increase your mobility. Start in your home and later outside
- Resume other normal household activities, for example, standing, sitting, and climbing stairs. Work on specific exercises several times a day to restore knee motion and knee strength. Although the goal is to perform the activities without help, you will have a physical therapist help you at home or a therapy center the first few weeks after surgery.
- Avoid sleeping with a pillow under your knee, as tempting as that may be. Rather sleep with pillows under your heel so that the knee gradually straightens as you sleep.
- During the day, focus attention on getting your knee fully straight and bending it beyond 90 degrees. Each day you should be able to bend it a few degrees more than the previous day.
Driving:
Most patients resume driving approximately 4 to 6 weeks after surgery.
You will likely be able to drive when your knee bends enough that you can enter and sit comfortably in the car. Furthermore, you will need to have enough muscle control to provide adequate reaction time for braking and acceleration.
Diet
After surgery, you may have a decreased appetite. An over-the-counter iron supplement and a balanced diet will help your wound heal and restore muscle strength.




Avoiding Problems After Surgery
Recognizing the Signs of a Blood Clot
Follow Dr. George Gendy’s instructions carefully to reduce the risk of blood clots
developing during the first several weeks of your recovery. Dr. George Gendy may recommend that you continue taking the blood-thinning medication you started in the hospital for approximately six weeks. Notify Dr. Gendy immediately if you develop any of the following:
Warning signs of blood clots in your leg. (DVT)
- Increasing pain in your calf
- New or increasing calf, ankle, and foot swelling
Warning signs of pulmonary embolism. (P.E.), when a blood clot has traveled to your lung:
- Sudden onset of chest pain
- Localized chest pain with coughing
- Sudden shortness of breath
Preventing Infection
One common cause of infection after total knee replacement surgery is from bacteria entering the blood from dentistry, urinary tract infections, or skin infections. These bacteria can seed your knee replacement.
After knee replacement surgery, patients may need to take antibiotics before dental work, dental cleanings, or surgical procedures that allow bacteria to enter the bloodstream.
Warning signs of infection. Immediately notify your doctor if you develop any of the following:
- Persistent fever (higher than 100.8 F orally) or Chills
- Increasing redness tenderness of the knee
- Drainage that looks milky or foul-smelling from the knee incision.
- Increasing knee pain with rest.
Avoiding Falls
A fall within weeks of surgery can damage your knee replacement and may result in more surgery. Stairs are a risk until your knee is strong and mobile. Assists devices such as a cane, a walker, handrails, or having someone help you until you have improved your balance, flexibility, and strength is recommended.
Your physiotherapist will help you decide what assist devices to use after surgery and when they can be stopped.
What To Expect
How A Knee Replacement Moves, Feels, & Sounds
The movement of your knee replacement after surgery can be predicted by the range of motion you had before surgery. Better knee motion is one goal of a total knee replacement, but the return of full motion is uncommon. Most patients can expect to nearly straighten and bend the replaced knee enough to get in/out of a car and climb stairs. Sometimes kneeling is uncomfortable but not harmful.
People will feel numbness around their incisions. You also may feel stiffness with deep knee bending activities.
It is normal to feel or hear the contact of the metal and plastic during bending or walking. With time, many people find them tolerable compared with the pain and limited function they experienced before surgery.
Your knee replacement may activate the metal detectors required for airport security. If the alarm is activated, tell the TSA about your knee replacement.
Protecting Your Knee Replacement
- Participate in physical therapy exercise programs to regain proper strength and mobility of your new
- Take appropriate precautions to avoid A leg fracture (bone break) may require additional surgery.
- Ask Dr. George Gendy about whether you need to take antibiotics before dental Notify your dentist about your knee replacement.
- See George Gendy periodically for a routine follow-up examination and x-rays. Dr. George Gendy will talk with you about the frequency and timing of these visits.
Extending the Life of Your Knee Implant
Approximately 90% of today’s total knee replacements function well 15 years after the surgery. In some cases, knee replacements have been seen to last as much as 30 years. Following Dr. George Gendy’s instructions, protecting your new knee and maintaining your general health are intelligent ways you can contribute to the final success of your surgery.
GEORGE GENDY’S TOTAL JOINT SURGICAL FAQ
BEFORE SURGERY
- Medications
- You will have a preoperative evaluation with your physician, where they will tell you which medications to hold on the morning of surgery. You will set this up.
- Aspirin: Baby aspirin (81 mg) daily is okay to continue. If you take a full-dose (325 mg) aspirin, this must be held for 1 WEEK before surgery.
- Medications to notify Dr. George Gendy’s team if you are taking:
- Anticoagulants (blood thinners) other than aspirin
- Immunosuppressive medications
- Over-the-counter anti-inflammatories are okay to continue. For example, ibuprofen (e.g., Advil or Motrin), acetaminophen (e.g., Tylenol), and naproxen (e.,g. Aleve).
- Discontinue Fish Oil supplements for 1 WEEK prior to surgery
- Opioids
- ALL opioid pain medications must be discontinued for at least 2 WEEKS prior to surgery.
- No opioids will be prescribed preoperatively.
- Dental Work (Before Surgery)
- You must avoid ANY dental work (including a routine dental cleaning) for 2 WEEKS before surgery.
- George Gendy prefers all planned dental work to be completed well prior to surgery unless it can be delayed 6 MONTHS after surgery.
- Nicotine
- ALL nicotine (i.e., cigarettes, cigars, nicotine patches, or chewing tobacco) must be discontinued for 6 WEEKS prior to and after surgery.
- George Gendy’s team will check blood nicotine levels prior to surgery.
- Medical Conditions
- Diabetes: Your hemoglobin A1C must be < 7.5 prior to surgery, or surgery will be canceled. Please optimize with the help of your primary care provider.
- Heart Conditions: These must be well-controlled prior to surgery, and you will need clearance from a cardiologist before you can proceed.
- Cardiac Stents: 1 YEAR without any complications is required before you can proceed with surgery.
- Other invasive cardiac procedures: It must be at least 6 MONTHS before you can proceed with surgery.
- Any other procedures: It must be at least 3 MONTHS before you can proceed with surgery.
- Please check with Dr. George Gendy’s service regarding the time frame after certain procedures, such as gastric bypass surgery or transplant surgery.
- Steroid Injections
- 3 MONTHS is required after a steroid injection into your surgical joint before you can proceed with surgery (opposite side is fine)
- Immunizations
- Related to your total joint, immunizations (including flu shots) are fine any time.
- Time of Surgery
- Our team will notify you when/where to report for your surgery a few days in advance.
- Allergies
- Please notify Dr. George Gendy’s team if you have a penicillin or latex
- Overall Health
- Inform Dr. George Gendy’s team of any cuts, scratches, rashes, or infections prior to your visit
- Inform Dr. George Gendy’s team of any colds or illnesses prior to your visit
- Inform Dr. George Gendy’s team of any dental issues prior to your visit
- All dental or skin infections must be completely treated prior to surgery
- All acrylic nails, gel nails, nail polish, are okay prior to surgery—do not need to remove.
AFTER SURGERY
- You will likely not see Dr. George Gendy; however, he will be notified of any medical emergency issues.
- You do need someone present for the surgery, and you do need to have a contact person available by phone. After surgery, you do need someone here when you are discharged if you are going directly home. If you are going to a rehabilitation center directly from here, Social Work will help you with transportation before your discharge.
- You will see Physical Therapy while in the hospital. They will direct your activity and give you recommendations upon discharge.
- For all primary replacements, you will be bearing weight on the day of surgery. This will be directed by Physical Therapy. If you have any gait aids (i.e., walker, crutches, cane), please bring them with you to the hospital.
- If it is not outpatient, the average stay in the hospital is 1 NIGHT.
- Disposition:
- If you have family or friends to care for you, you can be discharged home.
- If you require additional assistance, you may be discharged to a skilled nursing facility or home with home health care assistance. If you have preferences, please bring the contact information with you to the preoperative appointment.
- This decision will be made with social workers in the hospital
- Anticoagulation
- You will be on a blood thinner for six (6) weeks after surgery. Depending on your past medical history, this will be a full-dose aspirin twice daily
- Please bring your primary care provider’s name and phone number to the preop visit and contact them prior to your visit. You will need to follow up-up with them within one (1) a week of discharge from the hospital in all circumstances.
- Water
- Avoid submerging the incision in any water for 6 WEEKS
- Showering is permitted right away
- If the incision gets wet, pat dry.
- Sutures
- For primary and most revision replacements, sutures are under the skin and will dissolve on their own. Super glue placed on the incision will peel off on its own over the next 2 – 4 weeks.
- Dressings should be kept on for one week after surgery
- Compression Stockings
- We do not use compression stockings, but you may use them for comfort if you wish.
- Dental Work
- Avoid ANY dental work for 6 MONTHS AFTER surgery
- You will need antibiotic prophylaxis for at least one year before any invasive procedure, including ANY dental work. Please refer to the “Antibiotic Prophylaxis Card” that you will get from the service.
- Your dentist or primary care provider should provide the prescription for antibiotics. If they do not, Dr. George Gendy’s team can provide it for the 1st time only.
- Wait six months after surgery before having a colonoscopy
- Recovery
- You just had a major procedure. Recovery takes time (up to 1 year)
- Positions to Avoid
- Knee Replacement
- Avoid ANY kneeling for 3 MONTHS. George Gendy will instruct you otherwise at your 3-month follow-up visit.
- Driving
- You should not drive until you are able to ambulate ONLY using a cane and are not taking any narcotic pain medications. This is usually around 2 – 4 weeks.
- Most patients do not require a handicapped parking pass. If necessary, we will provide one for a maximum duration of 3 MONTHS.
- Follow-up
- George Gendy’s team will see you in approximately 3 WEEKS.
- George Gendy will see you in 4 MONTHS with repeat x-rays.
- Knee Replacement
Implants
During knee replacement surgery, Dr. George Gendy will resurface your damaged knee with artificial components called implants.
There are many different types of implants. The brand and design used by Dr. George Gendy or the hospital depend on the following:
- Your needs, your knee problem, and your knee anatomy, as well as your age, weight, activity level, and general health
- Dr. Gendy’s familiarity and experience with the device. The performance record of the implant
Dr. George Gendy will discuss the type of implant for your knee replacement surgery.
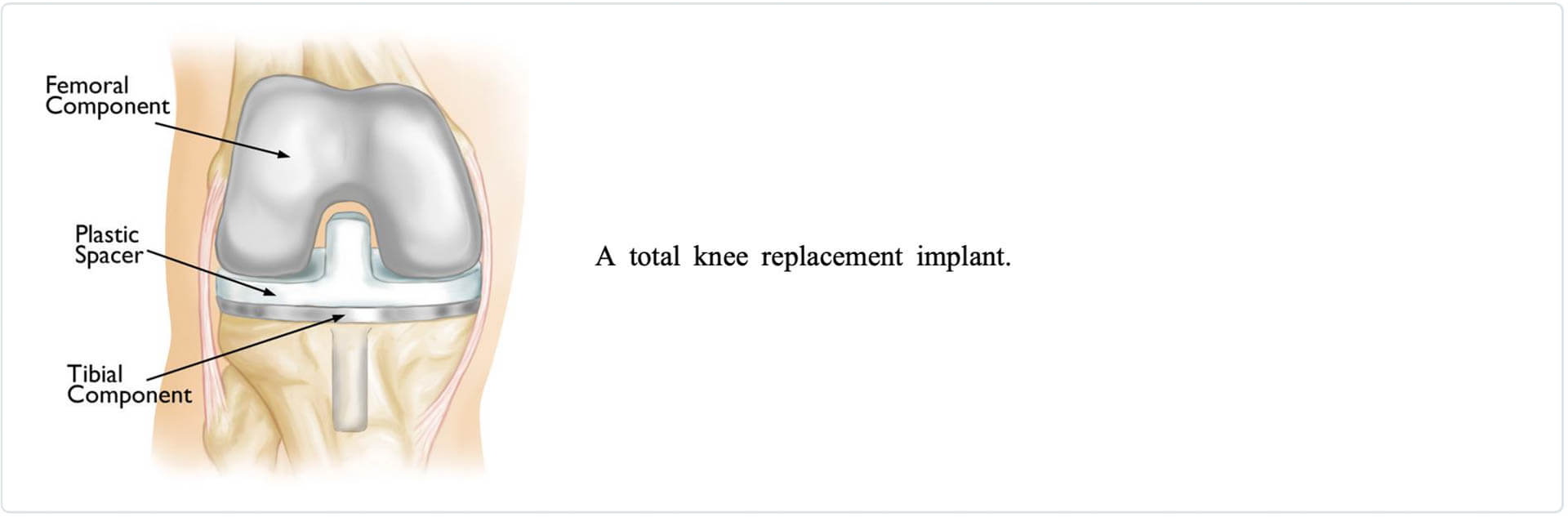
Implant Components
They are made of metal alloys, ceramic material, or durable plastic parts. Three bone surfaces are replaced in a total knee replacement:
The top surface of the This component is typically a flat metal platform with a resilient and durable plastic cushion, called polyethylene. Some implants do not have the metal portion and adhere the polyethylene directly to the tibia. For added stability, the metal component may have a stem that inserts into the tibia.
The lower end of the femur. The femoral component curves around the femur (thighbone). The groove allows the kneecap to move smoothly up and down as the knee bends and straightens.
The back surface of the patella. The kneecap component is a dome-shaped polyethylene that copies the shape of the patella (kneecap). In some cases, the patella is not resurfaced.
Engineers designed components so that metal always borders with plastic, providing smoother movement and minor implant wear.
Implant Designs
The knee is a “hinge” joint since it bends and straightens like a hinged door. However, it is much more complex because the bone surfaces roll and glide as the knee bends.
Modern implant designs recognize the complexity of the knee and replicate the motion of a normal knee. Healthy ligaments keep the joint stable in the knee. Some implant designs preserve the patient’s ligaments, while others substitute for them.
Gender-specific implants. Many manufacturers make knee implants, and there are more than 150 designs on the market today.
Many manufacturers have developed components for the end of the femur, which more closely match the average woman’s knee. However, no research to date shows that “gender-specific” implants last longer or provide better function than standard implants.
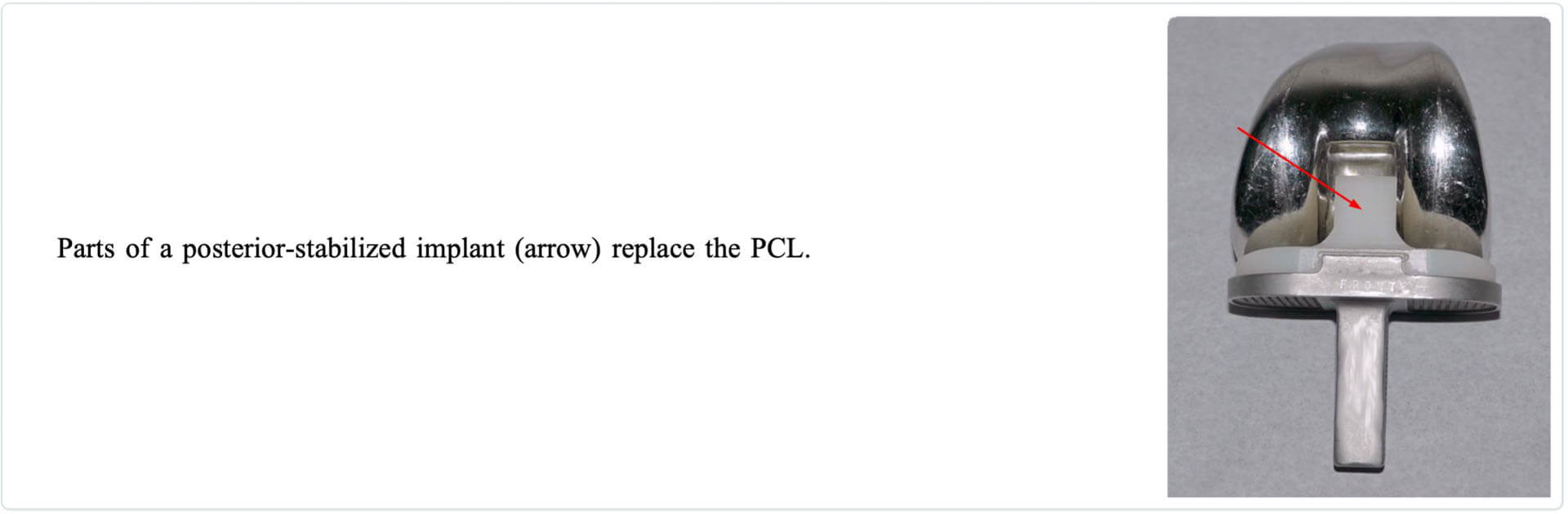
Posterior-Stabilized Designs
One of the most commonly used types of implant in total knee replacement is a posterior-stabilized component. This design removes the cruciate ligaments, and parts of the implant replace the posterior cruciate ligament (PCL).
The tibial implant has a raised surface with an internal post that fits into a unique bar (called a cam) in the femoral implant. These implants work together to do what the PCL does:
Stabilize the thighbone from sliding forward too far on the shinbone when you bend your knee.
Cruciate-Retaining Designs
Cruciate-retaining implants do not have the post and cam design. As the name implies, the PCL is kept with this implant design (the anterior cruciate ligament is removed). This implant is appropriate for patients whose PCL is healthy enough to continue stabilizing the knee joint.
Bicruciate-Retaining Designs
In most knee replacement procedures, the ACL is removed to allow for precise placement of the implant. In bicruciate-retaining designs, both the ACL and PCL are kept. This type of design is that the knee will function and feel more like a non-replaced knee by saving both ligaments.
Bicruciate-retaining components are newer to the market, and there are not yet many studies that show the pros and cons.
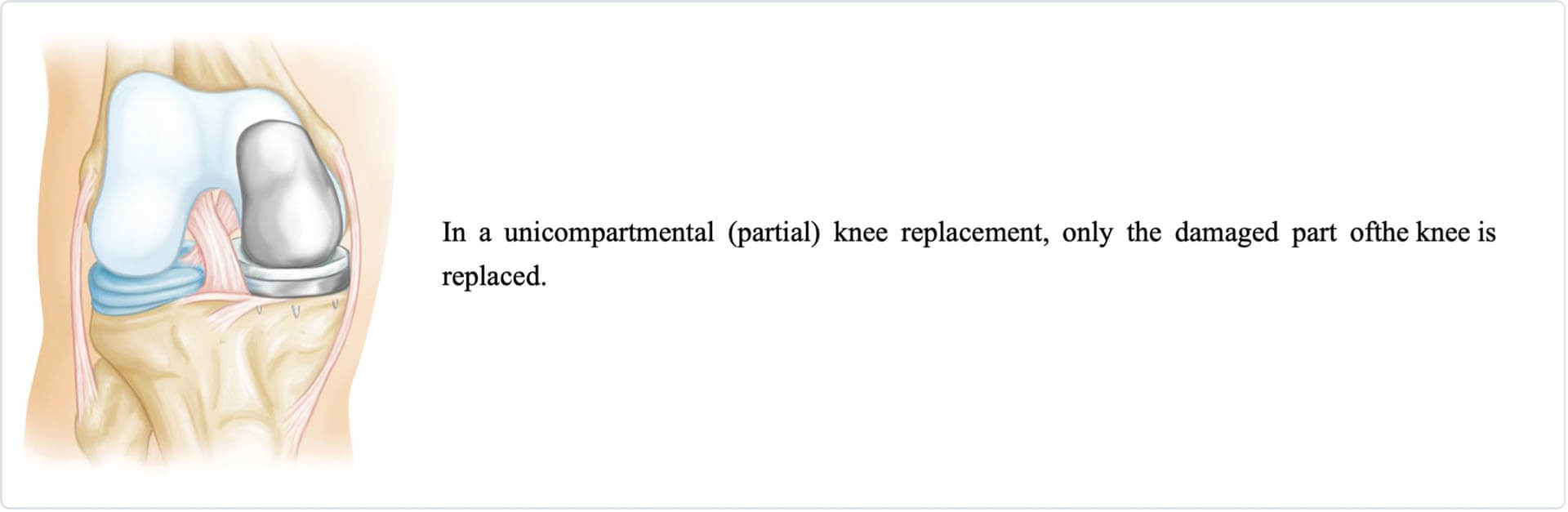
Unicompartmental Implants
While replacing the total knee joint is the most common procedure, some patients benefit from partial knee replacement.
If knee damage is limited to one part, smaller implants (unicompartmental knee replacement) resurface just that side.
Types of Tibial Implants
Fixed-Bearing Implants
The majority of patients get a fixed-bearing implant. In this design, the polyethylene (plastic) of the tibial attaches firmly to the metal implant underneath. The femoral part then rolls on this softened lining.Mobile-Bearing Implants
A mobile-bearing knee uses a polyethylene insert that rotates short distances inside the metal tibial component. This design allows patients additional rotation to their knee’s medial and lateral sides.Fixed- vs. Mobile-Bearing Implants
Durability. In some cases, excessive activity or body weight can cause a fixed-bearing prosthesis to wear out more quickly. Worn-out components can loosen from the bone and cause pain. Loosening is a significant reason artificial joints fail. Dr. George Gendy may recommend a rotating platform/mobile-bearing knee replacement in younger, more active, or overweight patients. Although these implants have been designed for long-lasting performance with minor wear, research has not shown improved durability or function with a mobile-bearing design. Soft-tissue support. Mobile-bearing knee implants require more assistance from soft tissues, such as the ligaments surrounding the knee. If the soft tissues are not robust enough, mobile-bearing knees can dislocate.Implant Materials
Implants are made of titanium or cobalt-chromium-based alloys. The plastic parts are made of ultra-high molecular weight polyethylene. Some are made of ceramics or ceramic metal mixtures. Regardless, implants weigh between 15-20 ounces.Material Criteria
The materials used must meet several criteria: The material must be biocompatible; it can be placed in the body without creating a rejection response. The material must be able to duplicate the knee structures they are replacing. They are strong enough to take weight-bearing activities, flexible enough to bear stress without breaking, and smooth enough to move against each other as required. The material must be able to retain its strength and shape for several years.Implant Fixation
There are different forms of fixation used to connect knee implants to bone.
Cemented fixation. The majority of implants are held in place with fast-curing bone cement (polymethylmethacrylate).
Cementless fixation. Implants can also be “press-fit” onto the bone. Press-fit fixation relies on new bone growing into the surface of the implant. These implants are made of metal that attracts new bone growth. Cementless components are textured or coated so that the new bone grows into the surface of the implant.
Hybrid fixation. Hybrid fixation is when the femoral implnat is inserted without cement, and the tibial and patellar components are inserted with cement.
Dr. George Gendy will evaluate your situation carefully before making any decisions regarding components and fixation. Feel free to ask what type of fixation will be used in your case and why that choice is appropriate for you.
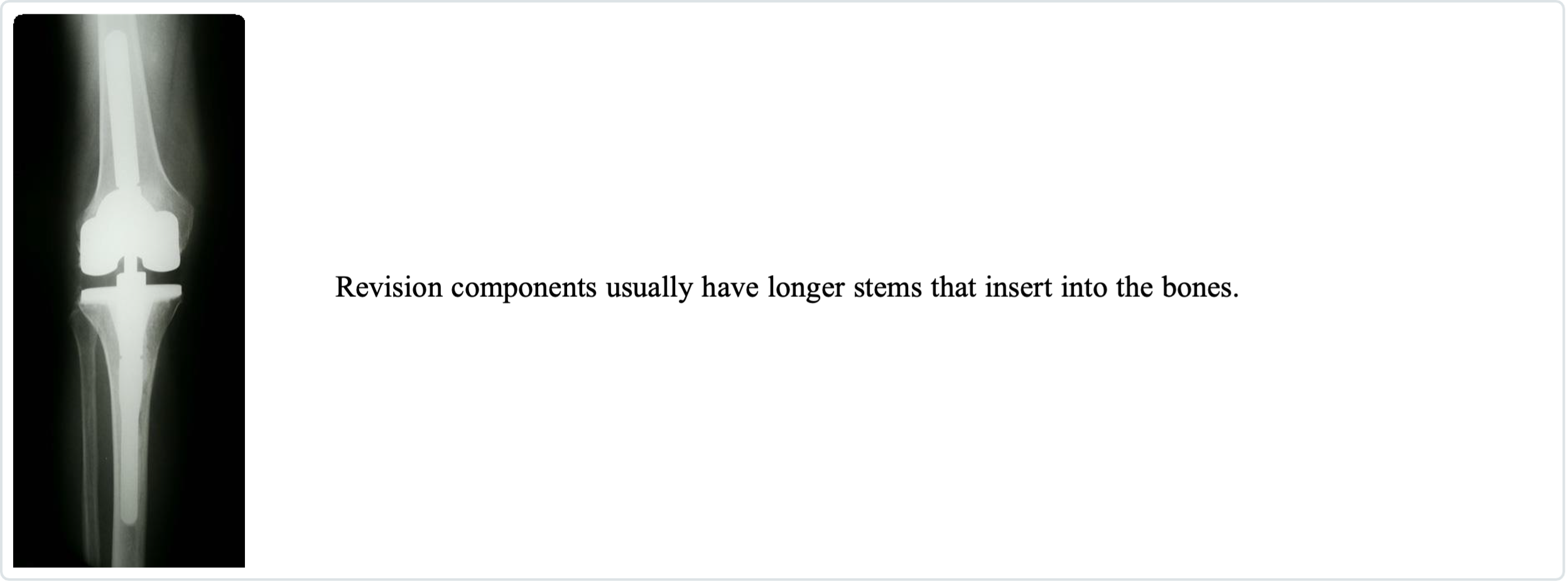
Revision Components
A knee replacement’s longevity depends on activity level, weight, and overall health. Similar to wear in the biologic joint contributed to the need for a replacement, wear in the artificial joint may eventually require a second surgery (called a joint revision).
A revision procedure is when parts of the original implant are removed and replaced with new components.
Revision components typically have longer stems that fit into the femur and tibia. They have metal pieces called augments to substitute for missing bone.
Revision components have a cam in the middle of the knee, similar to a posterior stabilized part. In revision components, though, the cam is more significant to increase stability.
When the knee is very unstable, the femur and tibia are joined with a metal “hinge” in the center.